AI’s Impact on Healthcare: Paving the Way Forward
Artificial Intelligence (AI) has the potential to completely change the healthcare industry. AI is poised to completely transform the healthcare industry by presenting previously unheard-of prospects for advancement. It includes tailored treatment plans and predictive analytics, and it promises major improvements in both patient outcomes and organizational effectiveness.

Unveiling Opportunities: AI’s Contribution to Healthcare Advancements
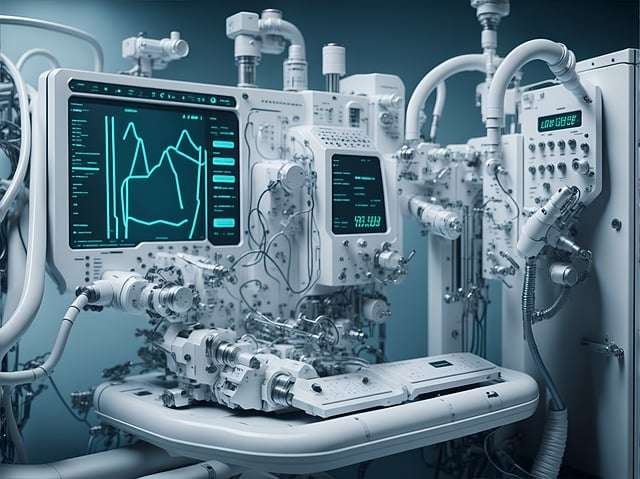
Across various healthcare domains, AI presents an extensive array of possibilities. AI offers a wide range of opportunities in the healthcare industry. AI-driven diagnostic technologies offer increased speed and precision, while predictive analytics can identify individuals at high risk and anticipate disease outbreaks. Robotic surgery devices also guarantee precise treatments, reducing mistakes and speeding up recuperation times.

Addressing Ethical Challenges: Navigating AI Implementation in Healthcare
The use of AI in healthcare raises ethical questions that need to be carefully considered despite its potential. Privacy concerns arise from the use of private patient information, which calls for strict security protocols. Furthermore, if the imminent threat of algorithmic bias is not sufficiently addressed, it may exacerbate already-existing healthcare inequities.

Encouraging Responsibly: Ethical Supervision of AI in Healthcare
Strong governance frameworks are essential for maximizing AI’s advantages while maintaining moral principles. AI decision-making procedures need to be transparent and accountable in order to maintain explainability and auditability of algorithms. In addition, promoting inclusion and reducing prejudice depend on giving justice and equality top priority in AI development.
Enhancing Patient Care
In addition to diagnostic precision, AI is revolutionizing patient care. AI-powered chatbots and virtual assistants provide round-the-clock support, answering queries and offering personalized health advice. Remote patient monitoring using AI algorithms enables early detection of health issues and timely intervention, improving patient outcomes and reducing hospital readmissions.
Streamlining Administrative Processes
Beyond clinical applications, AI streamlines administrative tasks, optimizing healthcare operations. Natural language processing (NLP) algorithms automate documentation processes, reducing paperwork and freeing up healthcare professionals to focus on patient care. AI-powered predictive analytics forecast patient admission rates, allowing hospitals to allocate resources efficiently and minimize wait times.
Safeguarding Patient Privacy
As AI systems analyze vast amounts of sensitive patient data, protecting privacy becomes paramount. Stringent data protection measures, such as encryption and anonymization, must be implemented to prevent unauthorized access or misuse of personal health information. Additionally, healthcare organizations must adhere to regulatory standards like HIPAA to ensure the confidentiality and integrity of patient data.
Mitigating Algorithmic Bias
Algorithmic bias poses a significant challenge to the equitable deployment of AI in healthcare. Biased datasets or flawed algorithms can lead to disparities in diagnosis and treatment, disproportionately affecting marginalized communities. To address this issue, AI developers must prioritize diversity and inclusivity in dataset curation and algorithm design. Continuous monitoring and auditing of AI systems can help identify and rectify bias, ensuring fair and equitable healthcare delivery for all patients.
Establishing Ethical Guidelines
To guide the responsible development and deployment of AI in healthcare, ethical guidelines and standards must be established. Multidisciplinary committees comprising experts in medicine, ethics, law, and technology can collaboratively draft comprehensive frameworks that balance innovation with ethical considerations. These guidelines should address issues such as consent, accountability, and fairness to ensure that AI benefits society without compromising ethical principles.
Enhancing Transparency and Accountability
Transparency and accountability are essential pillars of ethical AI governance. Healthcare organizations must be transparent about the capabilities and limitations of AI systems, providing clear explanations of how algorithms make decisions. Moreover, mechanisms for auditing AI algorithms should be implemented to detect and address errors or biases. By promoting transparency and accountability, healthcare stakeholders can build trust and confidence in AI technologies among patients and providers alike.
Promoting Diversity and Inclusion
Inclusivity should be a guiding principle in AI development to prevent the perpetuation of biases and disparities. Diverse representation in dataset collection and algorithmic training ensures that AI systems accurately reflect the demographics and healthcare needs of diverse populations. Additionally, healthcare organizations should prioritize cultural competence and sensitivity in AI applications to deliver equitable care to all patients, regardless of background or identity.
Investing in Ethical Education and Training
Education and training programs are vital for fostering a culture of ethical AI adoption among healthcare professionals. Healthcare providers must receive comprehensive training on the ethical considerations surrounding AI use, including data privacy, bias mitigation, and patient consent. Continuous education ensures that healthcare professionals remain informed about evolving ethical standards and best practices in AI governance, empowering them to make ethically sound decisions in their practice.
Collaborating Across Disciplines
Addressing ethical challenges in AI healthcare requires collaboration across disciplines and sectors. Multidisciplinary teams comprising healthcare professionals, ethicists, technologists, policymakers, and patient advocates can offer diverse perspectives and insights into complex ethical dilemmas. Collaborative efforts facilitate the development of holistic solutions that balance technological innovation with ethical imperatives, ensuring that AI benefits society as a whole.
Engaging with Stakeholders
Engagement with stakeholders, including patients, communities, and advocacy groups, is essential for fostering transparency, trust, and accountability in AI healthcare. Meaningful involvement of stakeholders in the design, implementation, and evaluation of AI systems promotes user-centered approaches that prioritize patient needs and preferences. By soliciting feedback and addressing concerns proactively, healthcare organizations can build consensus and foster public confidence in AI-driven healthcare solutions.
Advocating for Ethical AI Policies
Advocacy efforts are crucial for shaping policies that govern the ethical use of AI in healthcare. Healthcare organizations, professional associations, and advocacy groups can advocate for legislation and regulatory frameworks that promote transparency, fairness, and accountability in AI deployment. By engaging with policymakers and advocating for ethical AI policies, stakeholders can influence decision-making processes and ensure that regulatory measures align with ethical principles and societal values.
Fostering a Culture of Ethical Reflection
Finally, fostering a culture of ethical reflection and accountability within healthcare organizations is essential for ensuring ethical AI adoption. Healthcare leaders should encourage open dialogue about ethical considerations surrounding AI use and create mechanisms for reporting and addressing ethical concerns. By prioritizing ethical values and integrating ethical reflection into organizational culture, healthcare organizations can mitigate risks and promote responsible AI deployment that upholds patient safety, dignity, and autonomy.